Table of Content
Providers who have successfully navigated PDGM and are seeing positive returns from the updated payment model will actively seek agencies who were not as prepared for PDGM and are suffering from its effects. This event explores the strategies for deals, investments and transactions in the home health, home care, hospice and palliative care space. Yet because of the COVID-19 pandemic, any major recalibrations or corrections to PDGM’s foundation have, so far, been delayed, according to National Association for Home Care & Hospice President William A. Dombi. That could begin to change later in 2022, when CMS is gearing up to release its proposed payment rule for 2023.

For example, a recent stroke patient wants to be able to sleep in his or her own bed, which is upstairs. These are goals that the patient wants to achieve, and can be measurable and justifiable. Therapists should end the evaluation with summary of clinical assessment.
When did PDGM go into effect?
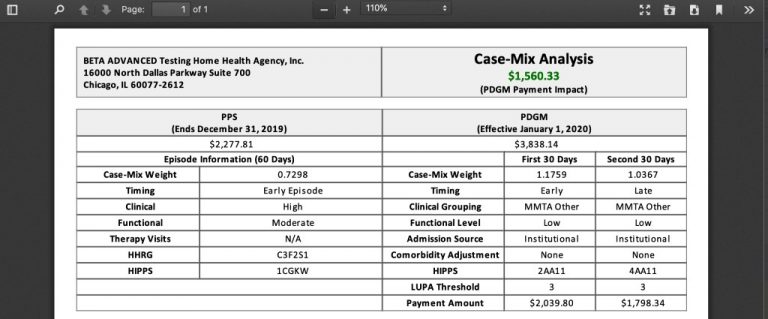
PDGM is a value-based care calculation- which means that agencies are given a certain amount of money and then the agency uses that money to provide the care needed for that patient. Effectively, CMS is saying "Agency, you have $X to do whatever you need to do for the patient, but you're not getting more than that, use it wisely." PDGM hopefully hasn't changed much for the patient. Hopefully the patient is still receiving what is needed to improve. PDGM also reduces the 60-day episode of care payment unit to thirty days.

HHA providers submit one RAP and one final claim for each 30 day period. Home health agency providers submit one RAP and one final claim for each 60-day episode. ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT-4 is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CDT-4.
HELPFUL PDGM BLOG POSTS
This lead to therapy overutilization and in some cases fraud. We have several blog articles that also explains PDGM for varioius parts of home health. CMS recognized the potential issue of therapy overutilization and/or fraud with therapy as a component of reimbursement.
As PDGM was rolled out and explained, many were understandably concerned with therapy and PDGM. There was concern about job losses, reduced pay, reduced work, layoffs, bankruptcies, and everything in between. A federal government website managed and paid for by the U.S. A .gov website belongs to an official government organization in the United States.
Patient-Driven Groupings Model Toolkit
However, an ‘other follow-up’ assessment is required when such a change would be considered a major decline or improvement in the patient’s hearth status. Home Care Answers makes things easy for agencies to know what the PDGM reimbursement will be along with the LUPA Threshold and HIPPS number on every chart in a simple report to review. We help provide vital information and maximize reimbursement by assuring accurate coding and OASIS.
Seeking partnerships within the industry in areas such as telehealth and coding could yield important gains for agencies struggling with adjustment. Referral sources will also play an important role particularly with regard to making sure coders are prepared for the new rules. CMS will be carefully watching the implementation of PDGM, with a special eye on how money is flowing to agencies. Home health agency billing departments should be evaluating and assessing their performance and understanding of the rules throughout this implementation. The decision-making on discipline/visit utilization should not change under PDGM. The plan of care should still be designed to meet the service needs of the patient.
People With Medicare
PDGM replaces the previous reimbursement model called Prospective Payment System which was implemented in 2000. ICD-10 Diagnosis Coding, OASIS Data, and Therapy Utilization. Centers for Medicare and Medicare Services used PPS for 20 years with updates along the way. Over time, CMS continued to issue guidance on important items in reimbursement- particularly diagnosis coding and therapy utilization. CMS wanted all along to have diagnosis coding be at the highest level of specificity and to use therapy for what the patient needed. Therapy over utilization and coding became problematic and PDGM was proposed several times over the years but finally was implemented January 1, 2020.
Low Utilization Payment Adjustments will also be analyzed with a far more scrutinized level of analysis. The Patient-Driven Groupings Model is the biggest change for home health agencies in over two decades. The transition to the new model requires agencies to examine patient needs, comorbidities, and referral sources to determine if their case mix optimizes reimbursement.
Coding and OASIS were derived to develop an effective score to show through data the condition of the patient at the time of assessment. To avoid LUPA there needed to be more than 4 and to stay under the radar, less than 20 therapy visits. Anything in between would not normally raise many questions. Naturally, many home health agencies and therapists would then provide as much therapy as possible in order to increase revenue for both the agency and therapist.
With the number of changes in store, inevitably some agencies will contest specific aspects of PDGM’s new requirements. In the past, CMS has already suggested PDGM isn’t budget neutral and is over-paying home health providers. Following 2020, CMS concluded that 2020 base payments were set 6% higher than they should have been. Going into 2020, nearly half of home health agencies planned to decrease therapy utilization, according to a mid-2019 survey conducted by NAHC ahead of PDGM implementation. The general concepts of medicare secondary payer billing will remain the same under PDGM.
Seamlessly supplement your clinical assessments with CareScout’s nationwide network of 35,000+ registered nurses. One of the biggest areas of PDGM that has been in the spotlight is in regard to therapy. That balancing act is even more important with PDGM, which must be budget neutral, as mandated by Congress.
Using this structure, a second period for a patient with a hospital inpatient stay during the period , in the Wounds group, high functional severity and no co-morbidity would be coded 4CC11. HIPPS codes continue to be reported with revenue code 0023. Case-mix adjusted payment for 60 day episode is made using one of 153 HHRGs based on severity levels. Two period timing categories used for grouping a 30-day period of care. Early episode of care - First two 60-day episodes in a sequence of adjacent covered episodes.

No comments:
Post a Comment